During a recent virtual fireside chat, I met with industry experts Courtney Hudson, President and Founder of Carebox; and Cyntha Griffo; Director of Communications and Education at the Abramson Cancer Center at the University of Pennsylvania, to discuss the current state of cancer trial matching, and learn more about how institutions can benefit from automated cancer trial matching. This post summarises the key takeaways from this insightful conversation.
Current challenges facing trial matching
Today, there’s no shortage of pent-up demand to match patients to relevant trials as early as possible. Hospitals are under pressure to enrol more patients into trials in order to speed the discovery and approval of new medicines. This is especially relevant in the oncology space, where medical breakthroughs can significantly improve outcomes for cancer patients.
Yet matching remains a largely manual and cumbersome process, with negative downstream impacts on both patients and academic cancer centers. Today, 80% of clinical trials fail to meet recruitment timelines and 25% of investigative sites fail to enrol enough patients. Fewer than one-third of clinicians discuss trial options during treatment planning, and less than 4% of US adults with cancer enrol in clinical trials, leaving an overwhelming number of families frustrated with the process.
Cynthia Griffo notes that in the course of her work at a large academic cancer center, she already works with community networks and satellites to fast track patients into trials. “But is it really fast?” she asks, “It would definitely be [more smoothly] handled with greater automation. It takes so much work to get to where we are. We have been talking for 20 years about this automation to the point of care. So, it's not really fast.”
Building a business case for automated cancer trial matching
A recent Inspirata survey on match rates revealed that the average cancer center seeks to increase patient enrolment in trials by approximately 75%. But with current enrolment rates averaging approximately half of this percentage, making a successful business case is imperative.
Highlighting the distinct financial and operational advantages of automation to hospital administration is a must. Having a good internal understanding of revenue per patient from clinical trials enables you to multiply that accrual in enrolment by revenue per patient in order to project what the technology is going to cost you over a period of time.
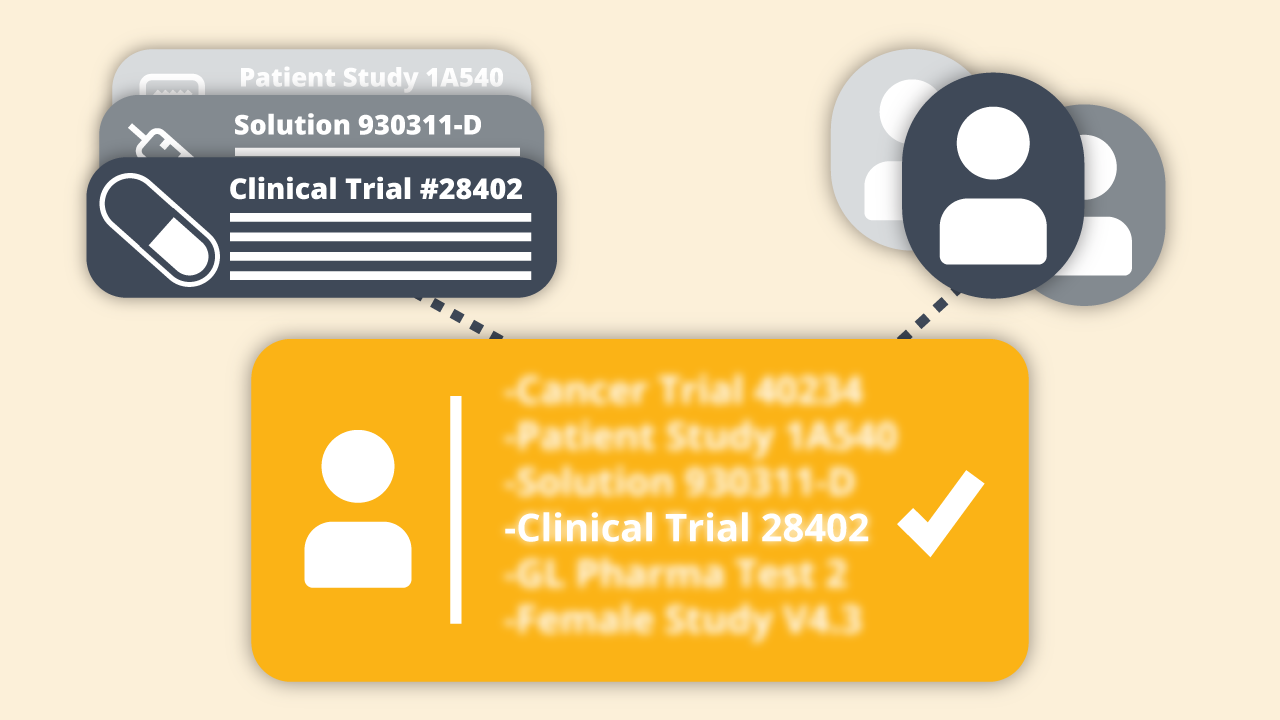
Operational benefits such as time savings are also important to quantify. Courtney Hudson notes that reducing the workload associated with identifying patients is the most immediate and obvious benefit of automation. “That's huge, it's just got to be less work, you can't do this stuff off the top of your head, both assessing all the patient variables, and all the trial variables for every arm of the study is just undoable.” Communicating how this translates into financial value to internal stakeholders is vital.
Ultimately, when a solution improves clinical research and patient care, it creates intangible benefits to the reputation of the institution and the community it serves. “For the Abramson Cancer Center, an improvement in automation would really allow us to further enhance our benefit to the community,” says Cynthia. “Our message has always been that the dramatic progress made in treating cancer has come from clinical trials. Consequently, patients who participate in trials gain access to the very latest changes in cancer care. To be able to turn this around more rapidly would provide a definite edge in a very competitive area where we are in Pennsylvania.”
Building a case for automating the clinical trial matching process requires a tailored, cross-functional approach due to the diversity of stakeholders.
Reducing the need to refer patients out; expanding patient options
Inspirata’s benchmark study also surfaced the frequency in which hospitals or trusts were required to refer patients to clinical trials outside of their institution. Sixty-nine percent of oncologists interviewed were required to refer patients out either occasionally or often. Automated matching of patients could potentially reduce the need to refer a patient out.
From Courtney’s perspective, access to accurate, instantaneous, sensible results greatly reduces friction in the matching process. First and foremost, physicians can not only view matches within their institutions or networks but can also view and offer regional or national trial matches. She provides an example: “While [the University of Pennsylvania] may get the inquiry, in fact, the patient lives closer to another NCI-designated cancer center that has the same trial open. So you can both figure out the logistics and the geography of where to make the referral to, as well as find anything you've got in-house. But you've got to have...those results be accurate; you need those results instantaneously.”
In addition to viewing the set of trials that are a match for the patient today, the ability to look ahead and provide informed patient treatment options based on precise, timely information that considers eligibility windows is appealing.
Courtney continues: “So you can see what's open today that's a match for the patient. Or...do a deeper dive into the trials we have open today...or that are open nationally, that have a particular biomarker requirement. And while the patient might be too early for that study...you can see that it's there as the next option you might tee up for the patient.” Providing the patient with a vision of what could come next, and prepping discussions on how to make informed decisions on treatments could be a true game-changer in patient care.
In the face of today’s challenging environment, automated cancer trial matching not only significantly reduces the manual burden on physicians or nurse coordinators, it also allows greater productivity to cover much larger sets of trials and patients. In addition, by potentially providing matches in real time—as the patient’s medical information is updated in the EMR—automation has the potential to change the doctor-patient dialogue, and massively increase enrolment of qualified patients into clinical trials, with direct positive impacts for improved patient care and approval of new medicines.
Inspirata would like to express our appreciation to our experts for sharing their insider perspectives on the challenges and opportunities facing cancer trial matching today. To watch the in-depth discussion, please fill out the form to view the webinar.
To learn more about the work Inspirata is doing in this area, please visit our Trial Navigator® solution's page.